Overview
A depressive episode isn’t simply “feeling down.” It’s a period of at least two weeks where mood, motivation, energy, sleep, and concentration fall below baseline—often with feelings of hopelessness or disconnection. Recognizing that these symptoms are part of an illness—not a personal failing—is the first step toward recovery.
Table of Contents
1) Recognize the Signs Early
Early recognition improves outcomes. Track changes in mood, sleep, appetite/weight, energy, interest, concentration, and physical symptoms. If symptoms persist beyond two weeks or impair daily life, schedule an evaluation. Validated tools such as the PHQ-9 or HAM-D help quantify severity and guide treatment.
- Mood: sadness, irritability, emptiness
- Sleep: insomnia or hypersomnia
- Appetite/weight: loss or gain
- Energy/motivation: fatigue, anhedonia
- Cognition: indecisiveness, slowed thinking
- Somatic: headaches, slowed movement
2) Rebuild the Foundation: Sleep, Nutrition, Rhythm
Sleep hygiene (and CBT-I if needed)
- Consistent sleep/wake times—including weekends.
- Avoid screens one hour before bed; keep the room cool and dark.
- If insomnia persists, CBT-I has robust evidence for improving sleep and mood.
Nutrition that supports the brain
- Don’t skip meals; emphasize whole foods and hydration.
- Include omega-3 sources(e.g., salmon, walnuts, flaxseed).
- Limit alcohol; it worsens sleep and mood regulation.
Move a little, daily
Even 10–20 minutes of brisk walking can increase serotonin and BDNF—key drivers of neuroplasticity also engaged by TMS and Esketamine.
3) Reframe Depressive Thoughts (CBT)
Depression amplifies cognitive distortions (e.g., all-or-nothing thinking, catastrophizing). Cognitive Behavioral Therapy helps you identify and reframe them:
| Depressive Thought | Healthier Reframe |
|---|---|
| “I’m a failure.” | “I’m struggling now, and I’ve succeeded before.” |
| “Nothing ever works out.” | “Some things haven’t worked; others still can.” |
| “It’s too late to change.” | “Change happens at every stage of life.” |
If doing this alone feels hard, that’s normal—structured therapy (CBT, interpersonal therapy, acceptance-commitment therapy) is effective and often covered by insurance.
4) Connection Is Part of the Cure
Depression isolates—but connection helps reverse the biology of stress and inflammation. Try:
- Text or call one trusted person today—no long update required.
- Schedule brief walks or coffees. Don’t wait until you “feel up to it.”
- Join a support group (in person or online).
Our team offers psychiatrist-led care with therapy, medication management, and advanced neuromodulation.
5) Evidence-Based Medical Treatments
Antidepressant medication
SSRIs/SNRIs(e.g., sertraline, escitalopram, venlafaxine) remain first-line for many. Taken consistently, they normalize neurotransmission and network function. Augmentation strategies (e.g., atypical antipsychotics, lithium, thyroid hormone) may be considered for partial response.
Transcranial Magnetic Stimulation (TMS)
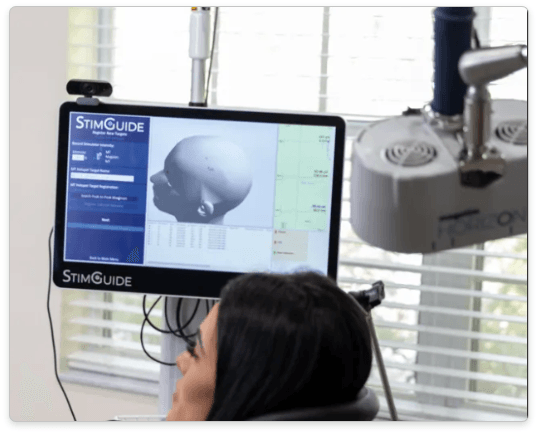
FDA-cleared, non-invasive TMS uses magnetic pulses over the left dorsolateral prefrontal cortex to re-engage mood circuits. At Florida TMS Clinic we use advanced 3D-guided navigation and modern protocols such as iTBS(≈3-minute sessions) and accelerated, high-dose formats (e.g., ONE-D/SAINT-style) discussed during evaluation to match patient goals and history.
- Medication-free and generally well-tolerated.
- Covered by most insurers after documented trials.
- Pairs well with therapy and medication for synergy.
Explore details: TMS in Tampa & Wesley Chapel.
Esketamine (Spravato®)
Esketamine nasal spray is indicated for treatment-resistant depression and for depressive symptoms in adults with MDD with acute suicidal ideation or behavior (with an oral antidepressant). It engages NMDA receptors, rapidly increasing synaptogenesis—often improving mood within hours to days.
- Administered on-site under monitoring, with an induction series and maintenance plan.
- Can complement TMS or medication management for durable benefit.
Learn more: Esketamine in Tampa & Wesley Chapel • Related: Esketamine for Anxiety & Esketamine for OCD.
6) Re-Engage Your Senses & Environment
- Morning light (10–15 min): stabilizes circadian rhythm and supports serotonin/Vitamin D.
- Nature micro-doses: a brief walk lowers cortisol and rumination.
- Mindfulness: 2–5 minutes noticing sounds, textures, and breath—no perfection required.
- Behavioral activation: schedule two small, meaningful activities daily.
7) Address Co-Existing Conditions
Depression often co-occurs with medical or psychiatric conditions. Ask your clinician about screening for thyroid disorders, anemia, sleep apnea, vitamin D/B12 deficiency, substance use, anxiety, and ADHD—treating these can accelerate recovery.
8) Have a Crisis Plan
9) Long-Term Prevention
- Continue therapy/medication or maintenance TMS as advised.
- Keep a steady daily routine; protect sleep.
- Use CBT skills and mindfulness during stress spikes.
- Schedule follow-ups—even when you feel better.
- Prioritize physical and social activity.
We personalize maintenance strategies (including brief TMS “boosters”) to preserve gains.
10) A Note of Hope
Recovery isn’t linear, but the brain is resilient. With today’s therapies—including TMS, Esketamine, and evidence-based psychotherapy—most people improve and reclaim their lives. If you’re ready for a plan tailored to you, we’re here to help.
Start Feeling Like Yourself Again
Our Tampa & Wesley Chapel teams provide precision-guided TMS, Esketamine, and comprehensive psychiatric care.
FAQ: Getting Out of a Depressive Episode
Is there a fastest way to feel better?
There’s no single “fastest” path for everyone, but behavioral activation, sleep stabilization, and prompt evaluation can shorten suffering. For treatment-resistant cases, TMS and Esketamine can accelerate relief.
Do I need medication if I’m already in therapy?
Not always. Many people recover with therapy and lifestyle changes. If symptoms persist or are moderate-to-severe, medication and/or neuromodulation can be added to improve outcomes.
Can TMS and Esketamine be combined?
Yes. They act through different mechanisms and can be complementary under psychiatric supervision, often improving speed and durability of response.
How do I know if I’m relapsing?
Watch for early warning signs: sleep disruption, loss of interest, irritability, fatigue, and negative thinking. Track with PHQ-9 and reconnect with your clinician early.
Educational content only. Not a substitute for individual medical advice. © Florida TMS Clinic.