TMS Therapy For Insomnia & Sleep Disorders
~ 5 MIN READ
This article will discuss the use of TMS therapy or Transcranial Magnetic Stimulation in treating insomnia and other sleep disorder. The neuromodulatory technique rTMS is a treatment method approved by the United States Food and Drug Administration for patients with major depressive disorder that has not responded to antidepressant medication. The device utilizes magnetic fields to generate localized electrical currents in neurons just a few centimeters below the scalp, creating depolarizing and normalizing effects. Localized brain stimulation impacts neural plasticity, activates compensatory processes, and influences cortical excitability. Additionally, rTMS has been used in various clinical trials to study and treat neurological and psychiatric disorders such as anxiety, post-traumatic stress disorder (PTSD), epilepsy. Several studies have found that Transcranial Magnetic Stimulation (rTMS) can benefit inefficiency and sleep quality.
Using magnetic fields to affect brain function is now being used to treat sleep disorders and multiple disorders associated with insomnia, such as Restless Leg Syndrome, Parkinson’s, Chronic Pain, or Anxiety. Many of our patients who are treatment-resistant depressed may have co-existing insomnia that may have preceded their depression or put them at risk of relapse. This symptom is often underappreciated and should be attended to improve outcomes., People who have insomnia may be at risk of developing depression and suicidal ideation, as reported by Suh et al. 2013. This is based on their 6-year follow-up study that documented two or more episodes of insomnia in 'nondepressed patients' increasing the risk of both depression and suicidal ideation. Studies have shown improvement in patients with primary insomnia when treated with TMS. Studies of both depression and insomnia scales may find that their findings can't be separated. However, they do document the need to be aware of both symptoms. There have been some conflicting findings of the effectiveness of treatment with TMS on insomnia.
Physicians and scientists have documented improvements in patients’ sleep with rTMS treatment. He et al. suggest that disturbed intracortical excitability is responsible for sleep disturbances such as insomnia, which causes a hyperarousal state of the cerebral cortex, affecting metabolism and hormones, enabling neurogenesis.
Clinical Evidence of TMS Efficacy for Insomnia
Sanchez-Escandon et. al. 2014 studied ten patients with idiopathic insomnia and EEG abnormalities who were given a series of treatment sessions using TMS over the left frontal and frontal central areas for ten days, leading to an improvement in total sleep time, sleep efficiency, sleep onset latency, total wake time, and wake time after sleep onset.
It was reported in Jiang et al. 2013 that rTMS improved both Slow Wave Sleep and REM sleep, compared to those who received CBT, or hypnotic agents. They reported that TMS had the lowest relapse rate and was a better option for insomnia than CBT. They studied 120 patients with chronic primary insomnia, assigning 40 people to receive rTMS, 40 people to take estazolam 2 mg, and 40 people cognitive-behavioral therapy focused on sleep health education and coping skills. The patients were treated with right dorsolateral prefrontal cortex transcranial magnetic stimulation (TMS) at 1 Hz for two weeks. Differences between the rTMS and other treatments were significant at three months after treatment, with improved stage three REM sleep and lab tests. This study shows that "rTMS treatment is better than medications and psychotherapy treatments in improving the sleep architecture." rTMS significantly decreased the body awakening level and provided a better long-term treatment effect.
Song et al. (2019) studied 20 patients with Primary Insomnia using 1 Hz rTMS for 14 days monitoring the Pittsburgh Sleep Quality Index, Insomnia Severity Index, and the Epworth Sleepiness Scale. They also conducted 20 minutes of TMS-EEG before and immediately after TMS. A PSQI, ISI, and ESS ratings showed significant improvements that were maintained for one month. The researchers found that targeting the right posterior parietal cortex through low-frequency rTMS for at least one month often reverses abnormal changes in the brain’s electroencephalogram and helps with Primary Insomnia.
Pellicciari et al. 2013 used ten daily bilateral rTMS treatments of 1 Hz over the right dorsolateral prefrontal cortex and subsequent 10 Hz TMS over the left dorsolateral prefrontal cortex in 10 patients with resistant depression. They used the Hamilton Depression Rating Scale and changes in sleep patterns with EEG changes during both NREM and REM sleep before and after rTMS. The topographical-specific decrease of the alpha activity during REM sleep over the left dorsolateral prefrontal cortex (L-DLPFC) was demonstrated. The study suggests that “rTMS, and specifically the high-frequency stimulation, can represent a relevant strategy in the modulation of hypoactivity syndromes, like in MDD. And they suggested that the left frontal alpha frequency of the REM sleep as a state-dependent marker for depression and its remission.”
Li et al. 2013 studied 30 patients with major depressive disorder and 30 patients with major depressive disorder associated with insomnia while following the Montgomery-Asberg Depression Scale and the Pittsburgh Sleep Quality Index; both groups improved after four weeks of treatment. People with insomnia saw improvements in their sleep quality, daytime functioning, and the amount of time they slept per day after treatment.
In a study by Khurshid and Holbert 2015, as early as day 2-the Insomnia Severity Index started to improve and significantly improved insomnia by session 5.
Tello et al. 2017 reported on 25 patients with chronic insomnia without depression who were given 20 sessions of 1 Hz rTMS at 110% MT for 1800 stimuli/day over the right dorsolateral prefrontal cortex and found 80% of them had a “significant decrease” in their Pittsburgh Sleep Quality Index with 32% relapse rate after six months.
Stultz et al. presented a poster in June 2019 at the SLEEP conference in San Antonio, Texas, on a 6-month study of insomnia, depression, and TMS. There was a significant improvement in their sleep in people with insomnia after they received dTMS delivered to the left dorsolateral prefrontal cortex at 120% MT for an average of 27 treatments. This benefit maintained itself for six months.
Theta Burst Stimulation for Insomnia
Mensen et al. 2014 calculated the effects of theta-burst stimulation on sleep and vigilance using both continuous and intermittent theta-burst protocols with inhibition or excitation of the left dorsolateral prefrontal cortex vs. the left dorsolateral associative visual cortex. Theta burst stimulation decreased the time it took to enter stage 2NREM sleep and increased sleep efficiency. It did not affect sleep drive or psychomotor vigilance of either form or location.
TMS & Insomnia & Comorbidities
Multiple reports of improvement in sleep while using repetitive transcranial magnetic stimulation to treat other disorders such as anxiety, restless leg syndrome, and chronic pain have been described.
TMS for Anxiety Plus Insomnia
With respect to anxiety, Osuna et al. 2018 studied 16 patients who underwent one session of excitatory rTMS to either the right DLPFC or left DLPFC. Results revealed that Right DLPFC rTMS treatment had the most improvement in sleep quality with an increase in an average time of sleep, decreased number of times eyes opened during sleep and improved sympathetic activity during sleep.
Huang et al. demonstrated the effect of 1Hz rTMS on a right-sided parietal cortex for patients with generalized anxiety and insomnia; their results showed improvement in the Hamilton Rating Scale for Anxiety and Pittsburgh Sleep Quality Index scores in 36 patients.
Diefenbach et al. 2019 measured the Insomnia Severity Index before and after Generalized Anxiety treatment with TMS over time. They used low-frequency (1 Hz, 90% MT, 900 pulses) to the right dorsolateral prefrontal cortex and documented elevated ISI scores pretreatment, subthreshold scores at posttreatment and non-clinical values at 3-month follow-up.
TMS for RLS Plus Insomnia
Restless Leg Syndrome can interfere with sleep because it is a significant source of insomnia, and treatment with TMS seems to improve sleep quality.
Altunrende et al. found that ten sessions of high-frequency rTMS over the supplementary motor area can help patients with restless leg syndrome improve their symptoms. a
Lin et al. 2015, using 15 Hz TMS at 100% MT to 14 patients with RLS over the leg representation motor cortex area of the frontal lobe, showed improvement in their IRLS-RS scores and the PSQI after only two weeks, followed by benefits lasting up to two months.
The research by Sanchez-Escandon et al. 2017 used left primary motor cortex TMS in a patient with periodic limb movements and restless legs syndrome, following IRLS-RS and PSG findings with 1 Hz/1000 pulses per day. They documented improvement in total sleep time from 342 minutes to 474 minutes, increased sleep efficiency from 70 to 80%, decreased periodic limb movements, and the patient reported subjective improvement in their sleep.
TMS for Chronic Pain Plus Insomnia
In a study conducted by Park et al., the improvement of insomnia severity from severe to sub-threshold increased in two women with lower back pain and chronic insomnia. The author used transcranial magnetic stimulation for three weeks, five days per week at 1Hz and1200 stimuli per session.
TMS for Parkinson Plus Insomnia
A growing number of studies suggest new ways to treat symptoms of Parkinson's Disease and help with sleep in those patients. Van Dijk et al. 2009 studied sleep with actigraphy and pressure data from a 5 Hz rTMS conducted over either the motor or parietal cortex in 13 patients with Parkinson’s disease. Research has found that rTMS over the parietal region but not over the motor cortex improved sleep efficiency and lessened episodes of nocturnal awakenings.
Antczak et al. studied 11 patients using 15 Hz rTMS bilaterally over both primary motor areas at 120% MT. They found that patients with Parkinson’s disease have an increase in NREM sleep spindles and decreased nocturnal arousal. Patients also report improvement by using this scale.
TMS for Substance Use Plus Insomnia
There has been much excitement about the treatment for substance abuse, and Lin et al. 2019 investigated sleep quality and mood in 105 male opioid addicts after an average of 6 months of abstinence. Forty patients were randomized to 10 Hz electroconvulsive therapy (ECT), and 40 were sham-treated. The other 25 participants did not receive treatment. The Pittsburgh Sleep Quality Index, Self-rating Anxiety Scale, and Self-rating Depression Scale found improved sleep quality, depression, and anxiety in dependent patients in early abstinence. This could have a beneficial impact on preventing future relapses.
TMS Plus Acupuncture for Insomnia
TMS has even been studied with acupuncture for chronic insomnia by Zhang et al. 2018. They studied 78 patients divided into two treatment groups of TMS and acupuncture vs. acupuncture with sham TMS. Both groups improved, but the control group improved more significantly.
Conclusion:
Multiple studies have shown that Transcranial Magnetic Stimulation (TMS) effectively treats insomnia but without a clear consensus on how to use it. There does seem to be great potential for growth in this area, and research is ongoing.
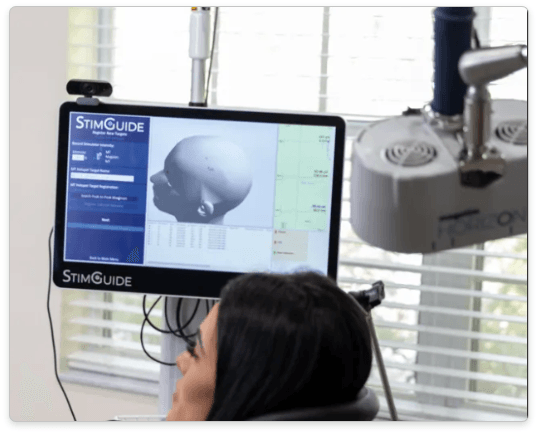
TMS for Insomnia at Florida TMS Clinic
Many of our patients with depression have comorbid insomnia. Based on what we know so far. We treat the underlying depression first with High Frequency Left DL-PFC TMS. We used the magnetic intensity of 120% MT for 3000 pulses. After ten sessions of treatment, we review the patient progress in depression, anxiety, and insomnia. If there is no improvement in anxiety and/or insomnia, we add Low-Frequency Right DL-PFC TMS to the treatment protocol. We usually magnetic intensity of 110% MT for 900 pulses and increase gradually to 1800 pulses if needed.
References
- Suh S, Kim H, Yang H-C, Cho ER, Lee SK, Shin C. Longitudinal Course of Depression Scores with and without Insomnia in Non-Depressed Individuals: A 6-Year Follow-Up Longitudinal Study in a Korean Cohort. Sleep. 2013;36(3):369-376. doi:10.5665/sleep.2452
- Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601-608. http://www.ncbi.nlm.nih.gov/pubmed/21532953.
- J Buysse D, F Reynolds C, H Monk T, R Berman S, J Kupfer D. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. doi:10.1016/0165-1781(89)90047-4
- Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens Insomnia Scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. 2000;48(6):555-560. doi:10.1016/S0022-3999(00)00095-7
- Chaudhuri KR, Pal S, DiMarco A, et al. The Parkinson’s disease sleep scale: A new instrument for assessing sleep and nocturnal disability in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2002;73(6):629-635. doi:10.1136/jnnp.73.6.629
- Walters AS, LeBrocq C, Dhar A, et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 2003;4(2):121-132. http://www.ncbi.nlm.nih.gov/pubmed/14592342.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540-545. doi:10.1093/sleep/14.6.540
- He Y, Sun N, Wang Z, Zou W. Effect of repetitive transcranial magnetic stimulation (rTMS) for insomnia: a protocol for a systematic review. BMJ Open. 2019;9(7):e029206. doi:10.1136/bmjopen-2019-029206
- Sánchez-Escandón O, Arana-Lechuga Y, Terán-Pérez G, et al. Transcraneal Magnetic Stimulation Improves Sleep Parameters in Patients Affected with Imsomnia Associated to Electroencephalographic Abnormalities. Neurosci Med. 2014;05(01):72-77. doi:10.4236/nm.2014.51010
- Arana-Lechuga Y, Sanchez-Escandon, Callado C., Castillo M., Gonsalez R., Jimenez-Anguiano A et al. Neurosci Med. 2011;2:178-184.
- Jiang C, Zhang T, Yue F, Yi M, Gao D. Efficacy of Repetitive Transcranial Magnetic Stimulation in the Treatment of Patients with Chronic Primary Insomnia. Cell Biochem Biophys. 2013;67(1):169-173. doi:10.1007/s12013-013-9529-4
- Pellicciari MC, Cordone S, Marzano C, et al. Dorsolateral prefrontal transcranial magnetic stimulation in patients with major depression locally affects alpha power of REM sleep. Front Hum Neurosci. 2013;7:1-11. doi:10.3389/fnhum.2013.00433
- HAMILTON M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62. doi:10.1136/jnnp.23.1.56
- Ishida, F.A., Kobayashi, A., Hu, A., Yamaguchi, T., Watahiki, H., and Kobyashi H. A Case Study: The Effect of Transcranial Magnetic Stimulation (TMS) on Stress Levels, Quality of Sleep, and the Autonomic Nervous System. Adv Clin Tranl Res. 2018;2(1).
- Li T, Wang W, Hong L, Lin Y, Wang F. Repetitive transcranial magnetic stimulation enhances sleep quality of patients with comorbid major depressive disorder and insomnia. Sleep Med. 2013;14:e303-e304. doi:10.1016/j.sleep.2013.11.743
- Montgomery, S., Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134(4):382-389. doi:10.1192/bjp.134.4.382
- Khurshid A., Holbert R. Rapid Improvement In Chronic Insomnia with Deep Transcranial Magnetic Stimulation (D TMS) In A Patient With Treatment Resistant Depression And Insomnia. Int J Innov Med Heal Sci. 2015;4:57-59.
- Tello A, Gerez M. Efficacy of rTMS to treat insomnia in patients without depression. Brain Stimul. 2017;10(2):498. doi:10.1016/j.brs.2017.01.455
- Khurshid, K. and Holber R. A New Approach to Treatment of Insomnia With Transcranial Magnetic Stimulation (TMS). In: San Diego, CA; 2017.
- Stultz DJ, Voltin R, Thistlewaite D, et al. 0401 Insomnia, Depression and Transcranial Magnetic Stimulation - A 6 Month Study. Sleep. 2019. doi:10.1093/sleep/zsz067.400
- Stultz DJ, Voltin R, Thistlethwaite D, Osburn S, Walton R, Burns T. Evaluating depression, weight change and insomnia with transcranial magnetic stimulation. Brain Stimul. 2018;11(6):e13. doi:10.1016/j.brs.2018.07.016
- Mensen A, Gorban C, Niklaus M, Kuske E, Khatami R. The effects of theta-burst stimulation on sleep and vigilance in humans. Front Hum Neurosci. 2014;8(JUNE). doi:10.3389/fnhum.2014.00420
- Mitler, M., Gujavary, K. and B. Maintenance of Wakefulness Test: A Polysomnographic Technique For Evaluating Treatment Efficacy in Patients With Excessive Somnolence. Electroencephalogr Clin Neurophysiol. 1982;53(6):658-661.
- Lin S, Hsiao Y-Y, Wang M. Test Review: The Profile of Mood States 2nd Edition. J Psychoeduc Assess. 2014;32(3):273-277. doi:10.1177/0734282913505995
- Huang Z, Li Y, Bianchi MT, et al. Repetitive transcranial magnetic stimulation of the right parietal cortex for comorbid generalized anxiety disorder and insomnia: A randomized, double-blind, sham-controlled pilot study. Brain Stimul. 2018;11(5):1103-1109. doi:10.1016/j.brs.2018.05.016
- Hamilton M. The Assessment of Anxiety States by Rating. Br J Med Psychol. 1959:50-55.
- Diefenbach GJ, Rabany L, Hallion LS, et al. Sleep improvements and associations with default mode network functional connectivity following rTMS for generalized anxiety disorder. Brain Stimul. 2019;12(1):184-186. doi:10.1016/j.brs.2018.09.004
- Altunrende B, Yildiz S, Cevik A, Yildiz N. Repetitive transcranial magnetic stimulation in restless legs syndrome: preliminary results. Neurol Sci. 2014;35(7):1083-1088. doi:10.1007/s10072-014-1653-4
- Lin YC, Feng Y, Zhan SQ, et al. Repetitive transcranial magnetic stimulation for the treatment of restless legs syndrome. Chin Med J (Engl). 2015;128(13):1728-1731. doi:10.4103/0366-6999.159344
- Sanchez-Escandon OA-LYT-PGV-MJ. Transcranial magnetic stimulation in sleep medicine. JSM Schizophr. 2017;2(2):1010.
- Park EJ, Lee SJ, Koh DY, Han YM. Repetitive transcranial magnetic stimulation to treat depression and insomnia with chronic low back pain. Korean J Pain. 2014;27(3):285-289. doi:10.3344/kjp.2014.27.3.285
- van Dijk KD, Møst EIS, Van Someren EJW, Berendse HW, van der Werf YD. Beneficial effect of transcranial magnetic stimulation on sleep in Parkinson’s disease. Mov Disord. 2009;24(6):878-884. doi:10.1002/mds.22462
- Antczak J, Rakowicz M, Banach M, et al. The Influence of Repetitive Transcranial Magnetic Stimulation on Sleep in Parkinson’s Disease. Biocybern Biomed Eng. 2011;31(3):35-46. doi:10.1016/S0208-5216(11)70017-1
- Chaudhuri, K.R., Pal, S., DiMarco, A., Whately-Smith, C., Bridman, K., Mathew, R., Pezzela, F. R., Forbes, A., Hogl, B., Trenkwalder C. The Parkinson’s disease sleep scale: A new insturment for assessing sleep and nocturnal disability in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2002;73:629-635.
- Zhang Y, Liao W, Xia W. Effect of Acupuncture Cooperated with Low-frequency Repetitive Transcranial Magnetic Stimulation on Chronic Insomnia: A Randomized Clinical Trial. Curr Med Sci. 2018;38(3):491-498. doi:10.1007/s11596-018-1905-2
- Zung WWK. A Rating Instrument For Anxiety Disorders. Psychosomatics. 1971;12(6):371-379. doi:10.1016/S0033-3182(71)71479-0
- ZUNG WWK. A Self-Rating Depression Scale. Arch Gen Psychiatry. 1965;12(1):63. doi:10.1001/archpsyc.1965.01720310065008
- Rosenquist PB, Krystal A, Heart KL, Demitrack MA, Vaughn McCall W. Left dorsolateral prefrontal transcranial magnetic stimulation (TMS): Sleep factor changes during treatment in patients with pharmacoresistant major depressive disorder. Psychiatry Res. 2013;205(1-2):67-73. doi:10.1016/j.psychres.2012.09.011
- Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): A psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573-583. doi:10.1016/S0006-3223(02)01866-8
- Rosenquist PB, McCall W V. Does rTMS treat insomnia? Brain Stimul. 2019;12(3):809. doi:10.1016/j.brs.2019.02.004
- Antczak J, Poleszczyk A, Wichniak A, Rakowicz M, Parnowski T. The influence of the repetitive transcranial magnetic stimulation on sleep quality in depression. Psychiatr Pol. 2017. doi:10.12740/PP/68503
- Soldatos CR, Dikeos DG PT. The diagnostic valididty of the Athens Insomnia Scale. J Psychosom Res. 2003;55(3):263-267.
- Arias P, Vivas J, Grieve KL, Cudeiro J. Double-blind, randomized, placebo controlled trial on the effect of 10 days low-frequency rTMS over the vertex on sleep in Parkinson’s disease. Sleep Med. 2010;11(8):759-765. doi:10.1016/j.sleep.2010.05.003
- Kaur M, Naismith SL, Lagopoulos J, et al. Sleep-wake, cognitive and clinical correlates of treatment outcome with repetitive transcranial magnetic stimulation for young adults with depression. Psychiatry Res. 2019;271:335-342. doi:10.1016/j.psychres.2018.12.002